Researchers leading the SWOG S1712 clinical trial have found that adding ruxolitinib to standard tyrosine kinase inhibitor (TKI) treatment for patients with chronic-phase chronic myeloid leukemia (CP-CML) significantly increased the percentage of patients who had a molecular response deep enough to warrant discontinuing treatment.
Results are being presented at the European School of Haematology’s 26th Annual John Goldman Conference on Chronic Myeloid Leukemia, to be held in Prague, September 27–29.
Kendra L. Sweet, MD, a SWOG investigator at Moffitt Cancer Center who was principal investigator on the S1712 trial will deliver the results Friday, September 27, as an oral presentation in the conference’s first scientific session, which is devoted to the meeting’s top-scoring abstracts.
“Treatment free remission has become a common therapeutic goal for patients with CP-CML. In spite of this, only approximately 40 to 50% of CP-CML patients achieve molecular responses that are deep enough to qualify them for an attempt to discontinue TKI therapy,” Sweet said.
“In this study the addition of ruxolitinib to TKIs resulted in significantly more patients with durable, deep molecular responses. Ultimately, this could lead to more patients successfully discontinuing treatment, which has been shown to significantly reduce health care costs and improve health-related quality of life.”
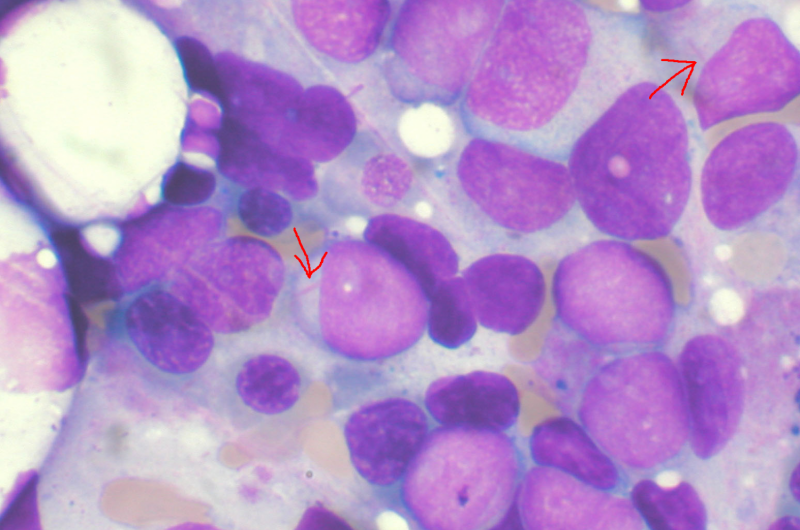
CML is often treated with a class of drugs known as tyrosine kinase inhibitors. But leukemic stem cells can hide from TKIs in a patient’s bone marrow. Preclinical data suggested that a drug called ruxolitinib can alter the bone marrow microenvironment to sensitize these stem cells to TKIs.
Researchers from SWOG Cancer Research Network hypothesized that adding ruxolitinib to TKI treatment would make TKIs more effective against leukemic stem cells, eradicating measurable residual disease in more patients.
In clinical trial S1712, they randomized 75 eligible patients with CML whose disease was still molecularly detectable on current therapy and who had been undergoing treatment with a TKI for at least one year. All patients continued their TKI treatment, but one half of patients also had the drug ruxolitinib added to their treatment.
After 12 months of on-study treatment, all patients had their blood tested for molecular response (MR), a highly sensitive test for RNA from a gene specific to leukemic cells. A score of MR4.0—considered a deep molecular response—indicates a reduction in this RNA to 0.01% or less of the baseline level. A score of MR4.5 indicates that no such RNA has been detected and is considered a complete molecular response.
The rate of S1712 patients scoring MR4.0 by 12 months was significantly higher on the ruxolitinib arm—46% versus 26% on the TKI-only arm. The rate of patients scoring MR4.5 at 12 months was significantly higher on the ruxolitinib arm as well—14% versus 3% on the control arm.
The addition of ruxolitinib also moved more patients to a remission deep enough that they were able to go off treatment. Two years after randomization, the proportion of patients who met the National Comprehensive Cancer Network (NCCN) guidelines criteria for being able to discontinue treatment was 29% on the investigational arm versus 11% on the control arm.
Toxicities were similar on the two arms. Two patients had grade 3 treatment-related adverse events (side effects) on the ruxolitinib arm. On the TKI-only arm, three patients had grade 3 treatment-related adverse events and one patient had a grade 4 adverse event. Grade 1/2 anemia was more common in patients treated on the ruxolitinib arm of the trial.
Sweet’s team is now working to characterize which patients with CML are most likely to benefit from having ruxolitinib added to their TKI treatment. The authors conclude that further trials are warranted to test whether this combination could increase the percentage of these patients who move to treatment-free remission.
More information:
A randomized trial of the addition of ruxolitinib to BCR::ABL1 tyrosine kinase inhibitors (TKIs) for patients with chronic myeloid leukemia (CML) with molecular evidence of disease (SWOG trial S1712).
Provided by
SWOG Cancer Research Network
Citation:
Clinical trial supports adding ruxolitinib to tyrosine kinase inhibitors for chronic myeloid leukemia (2024, September 23)
retrieved 27 September 2024
from https://medicalxpress.com/news/2024-09-clinical-trial-adding-ruxolitinib-tyrosine.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.


